Abstract
Background:
Sickle cell disease (SCD) is an inherited blood condition that predisposes affected patients to severe vaso-occlusive (VOC) pain events. The NHLBI (last revised in 2014) and ASH guidelines (last revised 2020) recommend a door-to-first dose should be within 60 minutes vs. 30 minutes from registration, and reassessment and re-administration of medications should be every 30 minutes. Non-IV routes of administration, i.e. intranasal (IN) can facilitate rapid analgesic treatment. Recent studies have shown IN Fentanyl as an effective pharmacological strategy to treat vaso-occlusive pain episodes.
Methods:
This resident-led Quality Improvement specific aim was to reduce the meantime from check-in to first analgesic delivery to SCD patients with VOC presenting to the Pediatric Emergency Department (PED) by at least 20% during 12 months and to improve the overall care of SCD VOC in accordance to best practices.
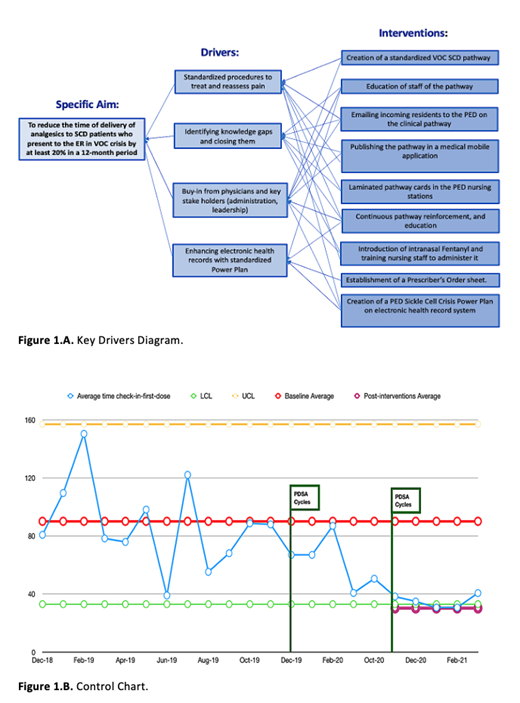
PDSA cycle methodology was utilized to identify root causes, countermeasures, and key drivers (Figure 1A). We implemented a SCD VOC clinical pathway for PED providers to utilize our enhanced and updated version of an electronic order set named "PED Sickle Cell Crisis Power Plan" that includes IN Fentanyl as first-line therapy for SCD VOC. IRB approval was obtained.
PED nursing staff was trained to administer IN Fentanyl with a nasal mucosa atomizer. Exclusion criteria of patients with SCD with other ICD-10 diagnosis codes, i.e pain not associated with VOC. The main indicators were assessment-to-dose time; registration-to-discharge time; first dose-to-discharge time, and rate of VOC admissions. Data was collected by discrete-time stamps and statistically analyzed using Excel 365. The analysis compared baseline with initial PDSA cycles from December 2019 to February 2020, and from September 2020 to March 2021.
Results:
From September 2020 to February 2021, a total of 54 encounters for SCD VOC qualified clinically to receive IN Fentanyl. A total of 49 of these encounters received this medication, while 5 refused its administration.
Patient demographics: Male-to-female ratio was 53% and 47%, respectively. The majority of the patients seen were adolescents (63% with ages between 12-21 years). African-American participants represented 88% and non-Hispanics 84%.
After our interventions, 94% of encounters have documented pain reassessment in their electronic medical records. IN Fentanyl was first introduced in the PED in September 2020, and became the first medication to be administered in 94% of the encounters. The average length of stay in the PED was 269 minutes (4 hrs. with 29 minutes).
The SCD VOC Clinical Pathway was used in 90% of the encounters and the SCD VOC Power Plan was used in 80% of them. From the total of encounters, 59% required admission to the floor for further pain management strategies.
As shown in the control chart (Figure 1.B), the meantime from check-in to first analgesic delivery to patients with VOC presenting to the PED was reduced to under 40 minutes by February 2021.
After the implementation of IN Fentanyl, there is an overall improvement of the waiting time for administration of medications of more than 70 minutes (from 138 min down to 67 minutes). Most importantly, 37% (18/49) of SCD VOC events were discharged after successful VOC pain management in the PED.
Discussion:
PED staff surveys demonstrated a lack of familiarity with current VOC guidelines and a standardized pathway. Medication refusal of IN Fentanyl was found to be related mostly to patient preference, poor knowledge about side effects, and parental fear for oversedation before our interventions.
Conclusion:
A multi-disciplinary team was formed to assist health care providers in the ED to deliver optimal care to patients with SCD based on the current evidence-based SCD VOC clinical pathway and efficient pharmacological intervention with IN Fentanyl.
Standardized procedures to treat and reassess pain for SCD VOC patients in the PED resulted in check-in to first-dose time reduction by 47%. There was a consistent improvement in Length of Stay in the PED, which decreased more than 60 minutes (from 5 hrs. 21 min. to 4 hrs. 29 min).
There is a significant improvement of quality in the care of VOC including 1. Pain scoring system. 2. Documented pain reassessment. 3. Use of a multidisciplinary reviewed protocol that includes PED SCD VOC clinical pathway, and an updated order set power plan with IN Fentanyl as the first line.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal